Swollen feet, also known as peripheral edema, can be a common complication of diabetes. Diabetes can affect the body in various ways, leading to fluid retention and swelling in the lower extremities. Here are some of the causes and treatment options for swollen feet in individuals with diabetes:
Causes:
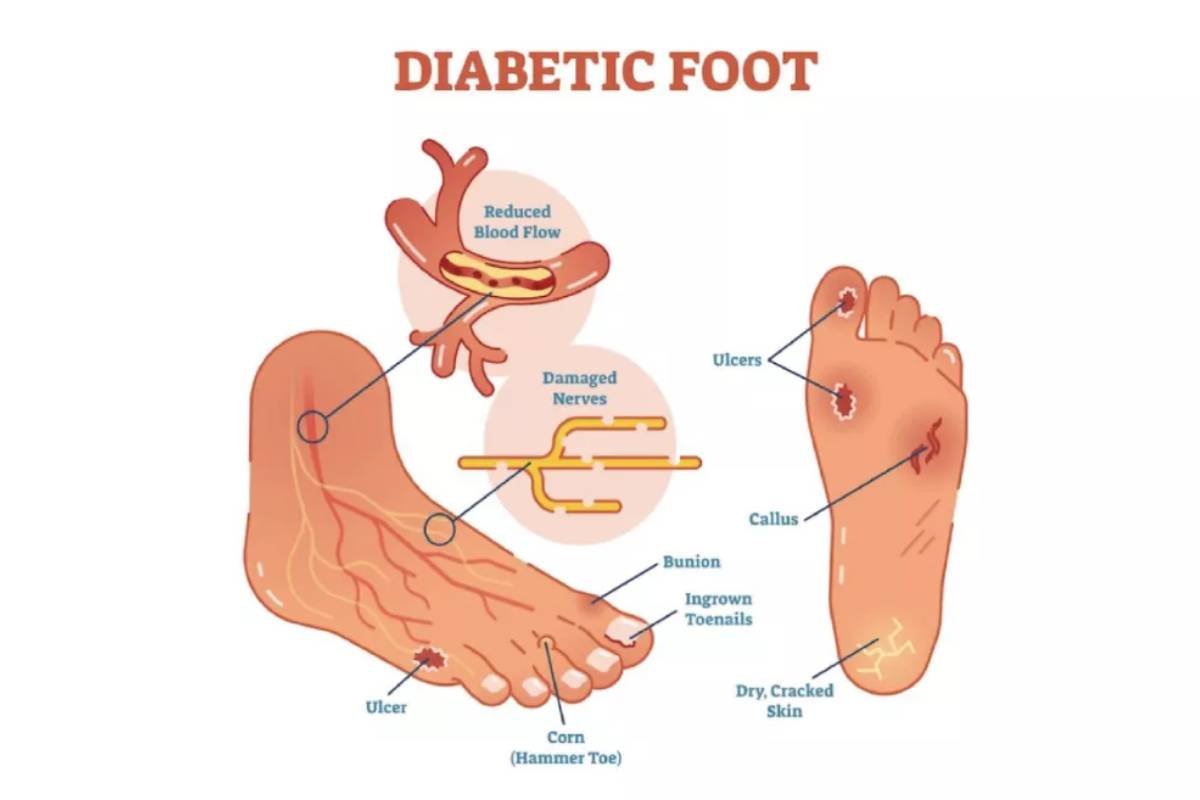
Poor blood sugar control: High blood sugar levels over an extended period can damage blood vessels and nerves. This damage can lead to reduced blood circulation and cause fluid to accumulate in the feet and ankles.
Neuropathy: Diabetic neuropathy is nerve damage that can affect the sensation and function of the legs and feet. This can lead to problems with regulating fluid balance and cause swelling.
Kidney disease: Diabetes is a leading cause of kidney disease, known as diabetic nephropathy. Kidney damage can affect the body’s ability to excrete excess fluids, leading to swelling.
Heart problems: Diabetes increases the risk of heart disease and congestive heart failure, both of which can lead to fluid retention and swelling in the lower extremities.
Medications: Some diabetes medications, such as thiazolidinediones, may cause fluid retention and edema as a side effect.
Treatment Options:
Blood sugar control: Maintaining good blood sugar control is essential. This involves monitoring blood sugar levels regularly, following a healthy diet, taking prescribed medications, and exercising as recommended by your healthcare provider.
Diet and sodium intake: Reducing salt (sodium) intake can help minimize fluid retention. A low-sodium diet can be beneficial in managing edema. Also, a balanced diet can help control blood sugar levels.
Medication adjustments: If certain diabetes medications are contributing to the swelling, your healthcare provider may adjust your treatment plan or prescribe alternative medications.
Compression stockings: These can help improve circulation in the legs and reduce swelling. Consult with a healthcare provider to ensure proper fitting and use.
Elevating the feet: Keeping your feet elevated above the level of your heart when resting can help reduce swelling by facilitating the return of fluid from the legs to the heart.
Regular exercise: Engaging in regular physical activity can improve blood circulation and help manage diabetes. Discuss an appropriate exercise regimen with your healthcare provider.
Diuretics: In some cases, healthcare providers may prescribe diuretics (water pills) to reduce fluid retention. However, these should be used with caution and under medical supervision.
Management of underlying conditions: If kidney disease or heart problems are contributing to the edema, it’s important to address and manage these conditions in conjunction with diabetes management.
Regular check-ups: Frequent monitoring of your condition and symptoms is crucial. Consult your healthcare provider for regular check-ups and adjustments to your treatment plan as needed.
It’s essential to work closely with your healthcare team to address and manage the specific causes of swollen feet in the context of your diabetes. They can tailor a treatment plan to your individual needs and provide guidance on lifestyle changes and medications to alleviate the swelling and its underlying causes





